CDC finds “nightmare bacteria” spreading across the country
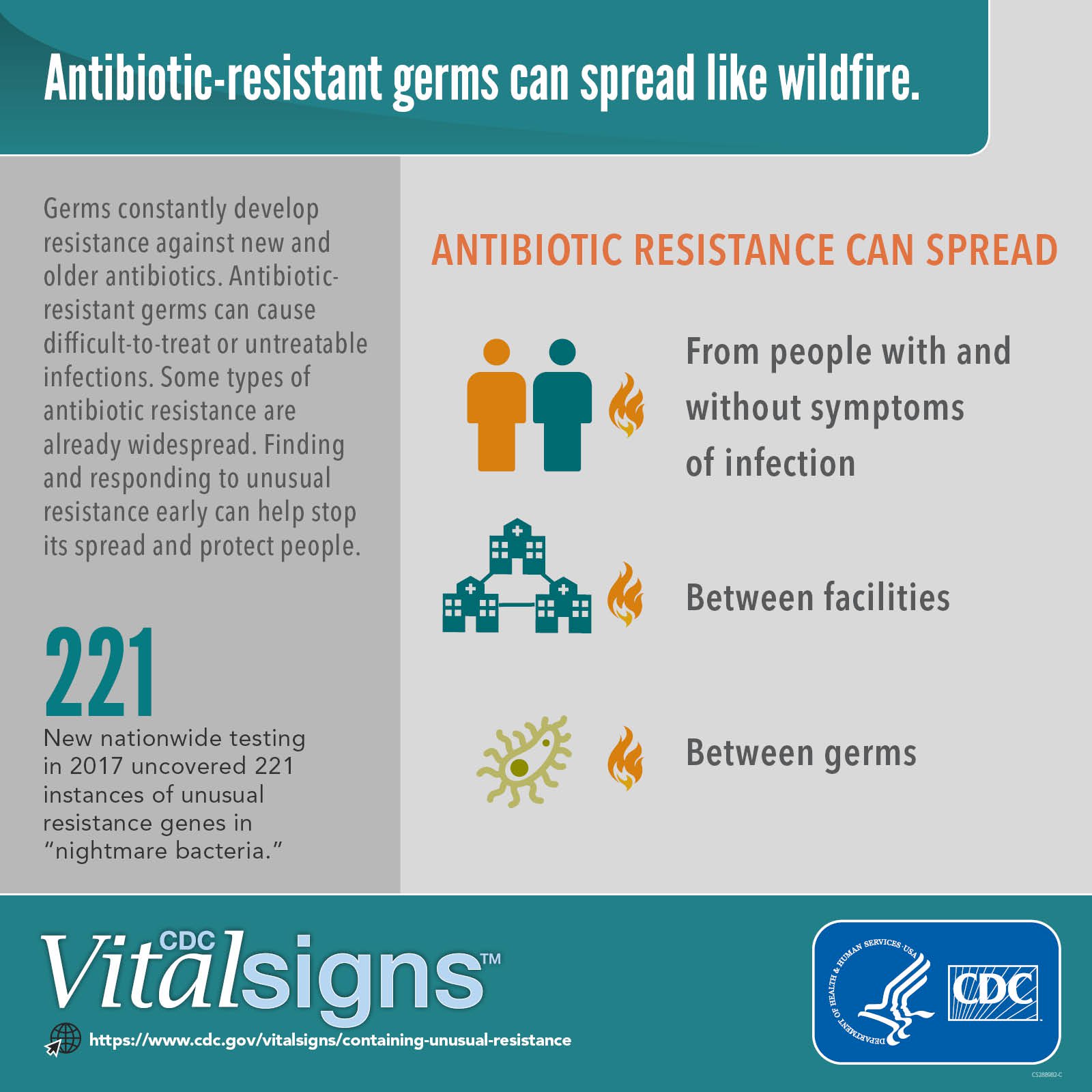
More than 23,000 Americans die each year from infections caused by drug-resistant germs, according to the CDC, and last year a first-of-its-kind nationwide study uncovered 221 instances of a rare antibiotic resistant (AR) “nightmare bacteria”. “Because the more you look, unfortunately, the more you find”.
This latest report, which the CDC published on its website, reveals that various different strains of antibiotic-resistant bacteria were discovered in 27 states, and were not all related to the same ailments. Although the report did not detail how many cases were fatal, Schuchat noted past research suggests “up to 50 percent can result in death”. The agency said it is working to keep resistance from spreading.
“This allows us to detect smaller resistance “fires” and “sparks” so they can be extinguished immediately”, Schuchat said, adding that the CDC supports more than 500 local staff across the country to combat antibiotic resistance when it emerges.
For the study, researchers tested more than 5,700 samples from across the country over the course of nine months. She emphasized that “unusual resistance may have spread to other patients and could’ve continued spreading if undetected”. Because “nightmare bacteria” are capable of spreading genes that make them resistant to most antibiotics, they can be untreatable or very hard to treat, said Dr. Schuchat.
It’s no secret that scientists are anxious about the spread of so-called “superbugs”-germs that are resistant to antibiotic treatment and therefore can not be easily stopped in their tracks”. After a threat is identified, the next step in the Centers’ strategy is containment: facilities working with the CDC’s AR Lab try to isolate infected patients as quickly as humanly possible, then initiate special procedures meant to root out any unknown infectees, as well as reduce or stop the pathogen’s spread to new patients. “CDC’s containment strategy calls for quickly identifying unusual resistance in patients, assessing infection control and the facility if unusual resistance is found”.
The paper recommends rapid identification of bacteria to check for resistance, completing infection control assessments, and testing those without symptoms who may also carry and spread the germs. In many cases, others in close contact with these patients also harbored the superbugs even though they weren’t sick – a risk for further spread. An aggressive approach to containing infections with odd resistance mechanisms works, Schuchat said.
The CDC has come up with a containment strategy to prevent the spread of the bug. It turned out that 1 in 10 people had what scientists call a “silent” infection, where they have the bacteria in their bodies but aren’t showing symptoms. And they do things like isolating the patient, making sure people wash their hands properly – so simple, so important.