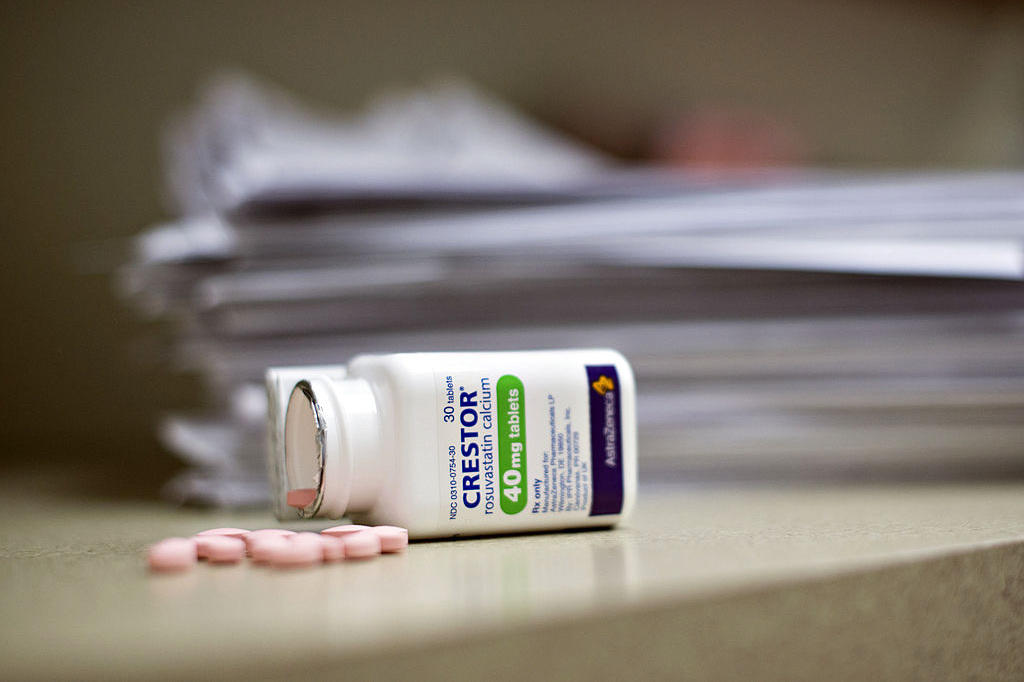
Doctors prescribe brand name drugs thanks to free meals
Response: Data released under the U.S. Sunshine Act reveals that in the last five months of 2013, over half of American physicians received free meals, gifts, or payments from the pharmaceutical industry.
The study highlights the subtle ways doctors may feel inclined to prescribe a drug after receiving just a small gift, even if the drug is more costly for patients and their insurance plans, the study authors said.
For the current study, a team of researchers led by Dr. R. Adams Dudley, a professor of medicine and health policy at the University of California, San Francisco, analyzed two US government databases from 2013.
A new study shows that even a single lunch offered by a drug company can bias a doctor’s decision on whether or not to prescribe a brand name drug. Doctors who received four meals courtesy of Allergan, the drugmaker behind Bystolic, were 540 percent more likely to prescribe the beta blocker.
R. Adams Dudley, MD, of UC San Francisco, and his coauthors linked to two national data sets to quantify the association between industry payments and physician prescribing patterns.
Drugmakers say their speaking programs provide a valuable educational service, and providing free meals-lunch in a doctors’ office, for example-gives physicians time to sit down and learn about new products from pharma reps. On the other hand, JAMA Internal Medicine editor-at-large Robert Steinbrook has raised a point that all are connected that includes revenue of health-care companies and independence of physicians. In part, that’s because the researchers acknowledge that they couldn’t determine whether the drugs were prescribed before or after doctors received meals paid for by companies.
Though the findings line up with other research on the subject, the authors note they can only show an association between financial incentives and a change in prescription habits, not a direct cause-and-effect relationship. The issue has resonated over the years as prices for prescription medicines rise, and many drug companies have paid civil and criminal fines for illegal marketing and kickbacks created to boost prescribing.
The study incorporated over 276,000 doctors and four different off-patent drugs, from four different pharmaceutical companies.
Plus, the rate of brand prescribing-measured as a percentage of a doctor’s scripts in that drug class-increased with the number of meals doctors accepted.
The study alone also can’t tell us whether these influences are necessarily bad – maybe doctors who grabbed a free meal promoting Pfizer’s antidepressant Pristiq walked away with a greater understanding of how to treat the condition. The other drugs in the study were prescribed less often.
Holly Campbell, a spokeswoman for the group, said the study “cherry-picks physician prescribing data for a subset of medicines to advance a false narrative” and doesn’t prove free meals influenced prescribing patterns.
In the assessment, the researchers have looked into meals, travel, speaking fee and other offerings between drug companies and doctors.
Previous studies have shown patients who are prescribed brand named drugs are less likely to stay on the full course or renew a prescription due to the cost with the opposite found for cheaper alternatives.
Here is a website where you can check out how much money drug companies spent on your doctors.
The possible link between perks for doctors and their prescribing behavior is troubling.
Before examining industry payments, the UCSF researchers first identified physicians from the 2013 Medicare Part D Prescriber file who wrote more than 20 prescriptions in any of four common drug classes.