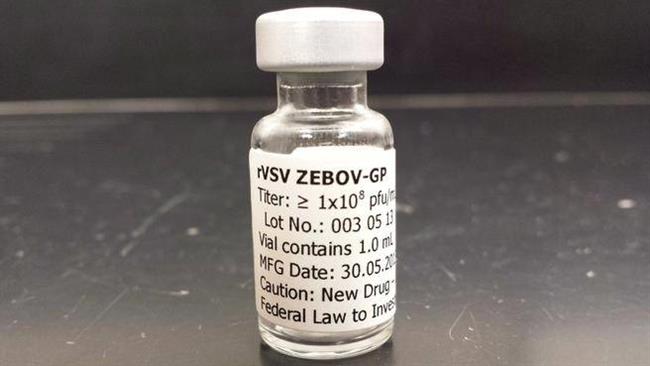
Ebola vaccine trial shows 100% effectiveness in Guinea
WHO’s announcement said while the vaccine has shown 100 percent efficacy in individuals, “more conclusive evidence is needed on its capacity to protect populations through what is called ‘herd immunity.’ To that end, the Guinean national regulatory authority and ethics review committee have approved continuation of the trial”.
Scientists have struggled for years to develop Ebola treatments and vaccines but have faced numerous hurdles, including the sporadic nature of outbreaks and funding shortages.
This, after the opposition groups urged their parliamentarians not to support any new government’s quarantine directive aimed to combat Ebola.
A vaccine against the deadly Ebola virus has led to 100 per cent protection and could transform the way Ebola is tackled, preliminary results suggest.
According to results published in the journal Lancet on Friday, the vaccine was found to be 100 percent effective in people treated.
World Health Organization (WHO) said the “remarkable” vaccine trial “could be a game-changer”.
There were no proven drugs or vaccines against the virus at the start of the largest outbreak of Ebola in history, which began in Guinea in December 2013. “In fact there was a vaccine that was brought to Sierra Leone whereby we tested it on our own frontline workers to see its efficacy”, said Bayraytay.
Texas was thrust into the crisis last year when Thomas Eric Duncan turned up at a Dallas hospital. A vaccine against the virus responsible would be of enormous value.
Soon after Duncan died of Ebola on October. 8, two nurses who cared for him, Nina Pham and Amber Vinson, were diagnosed with the virus. But, though new cases are now measured in dozens, rather than hundreds, a week, the disease has not been stamped out-and a new epidemic could flare up somewhere else at any time. Dallas was declared Ebola-free on November. 7.
“It’s really important to have a tool against these infectious diseases and to stop the ongoing outbreak in Guinea and Sierra Leone”, he said.
This strategy, known as ring vaccination, was also employed to eradicate smallpox in the 1970s.
“We hope that with this discovery, the stigma that we have had to deal with and the fear of this illness will end”, Keita said, while adding that existing measures aimed at preventing the virus would remain in place.
“By this time we were thinking that this vaccine would have been up and running, and that people would have been benefiting from it already.” said Yumkella.
Jeremy Farrar, a leading infectious disease specialist and director of the Wellcome Trust, said the trial “dared to use a highly innovative and pragmatic design, which allowed the team in Guinea to assess this vaccine in the middle of an epidemic”.
As data began to emerge showing the very high protection rates in those vaccinated immediately, however, researchers decided on July 26 that they would no longer use the “delayed” strategy, since it was becoming clear that making people wait involved unethical and unnecessary risk.
Because no placebos were used, volunteers knew whether they had received the vaccine, which could have influenced the study’s outcome.
WHO officials say early results were so promising that random tests were stopped this week so everyone at risk could receive the vaccine immediately.